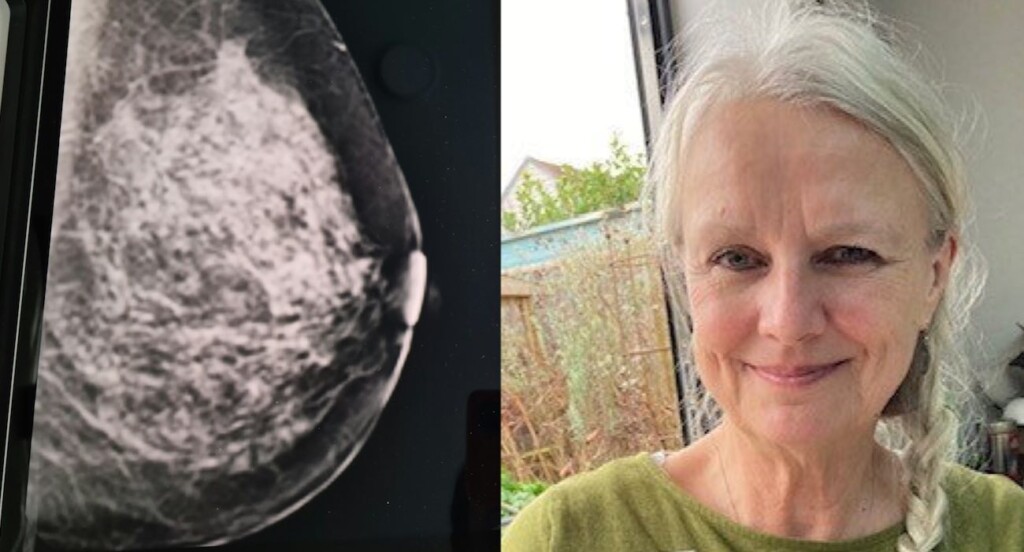
 (Left) cropped image by Getty images / Unsplash+ (right) Sheila Tooth via SWNS
(Left) cropped image by Getty images / Unsplash+ (right) Sheila Tooth via SWNSArtificial intelligence successfully detected a woman’s breast cancer, after a routine scan evaluated by humans came back as ‘normal’.
Sheila Tooth was given the all-clear after her most recent mammogram was examined by two experienced radiologists who determined that there were no signs of cancer. However, University Hospitals Sussex, where she had her appointment, was participating in research to see if AI could improve early detection.
The technology spotted cancerous cells which were undetectable by the human eye, which allowed Sheila, who had been diagnosed with early breast cancer 15 years ago, to get minimal treatment as early as possible.
“It’s extraordinary and I’m amazed,” said the retired nurse from West Sussex, England. “I knew that whatever they could see on my scan must have been incredibly small if it wasn’t picked up the first time.”
The mother-of-one was diagnosed with the same early non-invasive breast cancer as before—but because it was found so early, she was able to have a lumpectomy and didn’t need any further treatment.
Now, recovering from the surgery, she says she is so grateful for the AI technology.
“When I talk to friends, we just can’t believe this AI can detect what the human eye can’t always see. I just feel so lucky.
“Being 68, this may have been my last mammogram, so my early cancer might have developed into invasive cancer in my 70s, so, I’m deeply grateful for it to have been caught so early.”
EXCITING NEWS: Manuka Honey Reduces Breast Cancer Cell Growth by 84% in Human Cells and Mice
Five out of 12,000 ‘normal’ screenings were overturned
University Hospitals Sussex is one of 15 trusts across the UK that participated in the project to test if AI can spot cancers humans may miss. The project used an AI system developed by Kheiron Medical Technologies called Mammography Intelligent Assessment, and was funded by the NIHR and NHS England.
Throughout the two-month project, more than 12,000 mammograms deemed to be normal by radiologists were reviewed using the AI system, which suggested that just under 10 percent of those films should be re-read by a clinical panel to identify any potential cancers that were not detected in the initial screening.
Upon further review, 11 women were asked to come back for investigation. Five of these were found to have breast cancer.
Dr. Olga Strukowska, a consultant radiologist and director at the West Sussex Breast Screening Program, said we are still in the early stages of AI evaluation in clinical scenarios but based on current trials and research, AI will surely find a place in screening programs.
AMAZING AI: New AI Smartphone App Accurately Diagnoses Ear Infections and Prevents Unnecessary Antibiotic Use
“The earlier and more accurately we detect cancer, the better the chance our patients will have a positive outcome. That’s why this is so exciting.
“It empowers screening services to deliver confident, accurate, timely results through deep learning technology that works with radiologists and promotes high-quality standards of care for our patients.”
Steve Dixon, Senior AI Project Lead for Breast Services, said, “I have no doubt that, in time, integrating AI with clinicians’ expertise will enhance the effectiveness of patient care, improving both outcomes and the quality of service for patients.”
University Hospitals Sussex is now planning to take part in a national randomized controlled trial involving AI – which forms part of the next phase of introducing the technology to breast cancer screening.
MORE BREAKTHROUGHS: Hand-held Test for Breast Cancer Uses Your Saliva and Gives Accurate Readings in 5 Seconds
Mammogram patients need to be registered with a doctor to be invited for the added breast cancer screening, but Sheila now recommends the technology to everyone, saying, “It’s just fantastic!”
SPREAD THE GOOD NEWS By Sharing on Social Media…
Source link

