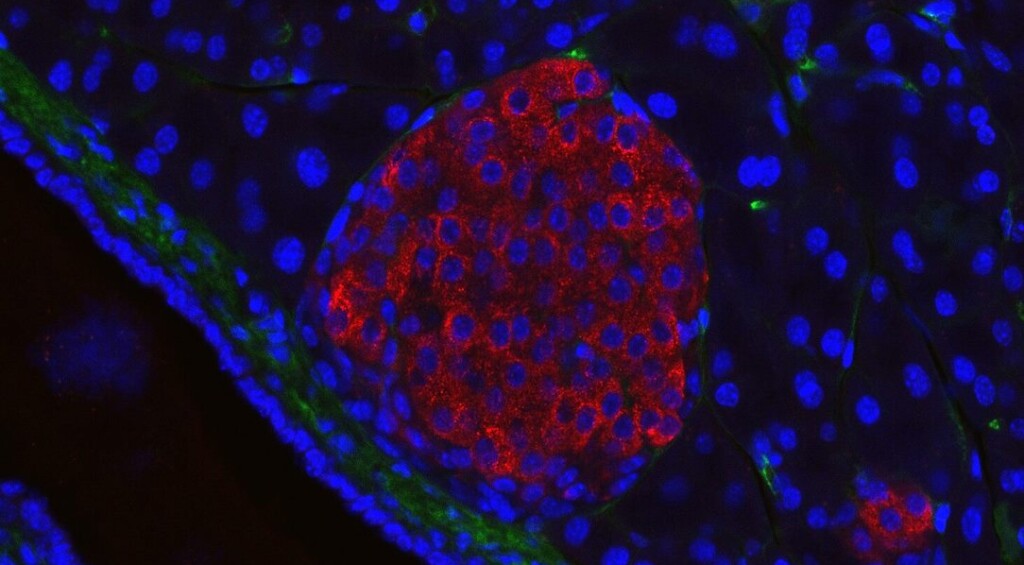
 A mouse pancreatic, or islet cell, with the red color marking the insulin – Jakob Suckale, CC 3.0. BY SA
A mouse pancreatic, or islet cell, with the red color marking the insulin – Jakob Suckale, CC 3.0. BY SA“I can eat sugar now,” said a woman from Tianjing, China, who recently became the first human to have their type-1 diabetes cured through a stem cell procedure.
Using the patient’s own stem cells, the results offer hope of limitless treatment options for type-1 diabetes, where special insulin-producing cells were previously needed from a donor.
Unlike type-2 diabetes which can be developed through poor diet and lifestyle choices, type-1 diabetes develops on its own in certain humans.
Type-1 diabetes is classified as an autoimmune disorder, as the immune system attacks islet cells in the pancreas responsible for producing insulin, a vital metabolic signaling hormone that instructs muscle tissues to absorb excess glucose and other sugars out of the bloodstream.
Treated with exogenous insulin and a mixture of immunosuppressants, the only thing like a cure is an islet-cell transplant, for which there are not anywhere near enough donors to meet the demand.
Instead, Chinese researchers reverse-engineered the patient’s own tissues to produce pluripotent stem cells which they then chemically reprogrammed to form islet cells. Once transplanted, the researchers, whose first subject was a 59-year-old man, observed he was producing his own insulin within 3 months, and after 4 months had a glycemic range that was 98% similar to that of a non-diabetic.
James Shapiro, a transplant surgeon and researcher at the University of Alberta in Edmonton, Canada, told Nature press that the results of the surgery are stunning. “They’ve completely reversed diabetes in the patient, who was requiring substantial amounts of insulin beforehand.”
In this more recent case of the young woman, the cultivated stem cells were injected during the surgery into the abdominal muscles—a new introduction site for this procedure. Previously, donor islets were transplanted into the liver, where they couldn’t be observed.
By contrast, in the abdominal tissue, the islet cells’ activity could be monitored with an MRI machine.
YOU MAY ALSO ENJOY: Lab-Grown Blood Stem Cells Could Replace Bone Marrow Donations for Transplants
Two-and-a-half months later, she was producing enough insulin to live without needing top-ups, and she has sustained that level of production for more than a year.
“That’s remarkable,” said Daisuke Yabe, a diabetes researcher at Kyoto University who wasn’t involved in the study. “If this is applicable to other patients, it’s going to be wonderful.”
SIMILAR NEWS TO THIS: Experimental Type 1 Diabetes Drug Shields Pancreas Cells from the Usual Crippling Immune System Attack
In the woman’s case, she was already taking immunosuppressants for a previous liver transplant, and so the researchers can’t confirm whether or not the new islet cells would be subject to the same autoimmune response as before.
Generally, medical researchers want to see years pass by of normal function before acknowledging that “curing” took place. The woman will reach the two-year mark in November. If she is still experiencing normal glycemic activity, cell biologist and lead author of the research Dr. Deng Hongku at Peking University Beijing, wants to expand the trial to between 10 and 20 people.
SHARE This One-Of-A-Kind Result In Battling This Dangerous Disease…
Source link

